Interview: Dr. Ritchie Shoemaker, MD, When Antibiotics Don’t Work
November 9, 2007 in Interviews by Sue Vogan, with Dr. Ritchie Shoemaker, MD
"At the end of the day, have we done our jobs as physicians in all aspects of these illnesses?" Dr. Ritchie Shoemaker is trying, in his practice, to make sure the answer to this question is "yes." Is it only Lyme disease ailing us? If we have been on antibiotics and still aren't getting better, could there be something that has been overlooked - like a biotoxin?
Sue: What is a biotoxin?
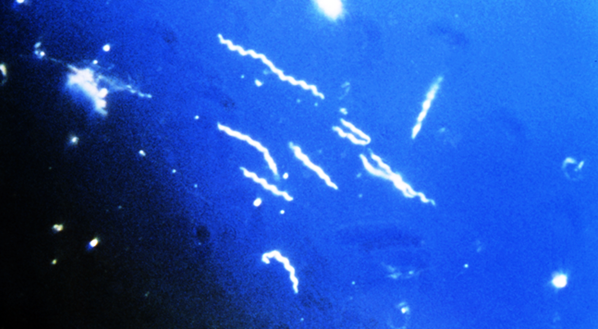
Dr. Shoemaker: Living organisms produce biotoxins. These biotoxins are small compounds made by living creatures. However, neurotoxins go from cell to cell and bind to particular types of receptors. Once done, a biological effect is started. One toxin will set off ten inflammatory cascades or results and that ten each sets off ten more, and soon - all very rapidly.
Sue: What is a microbacteria?
Dr. Shoemaker: Tuberculosis is one kind of a microbacteria. The importance of this is that microbacteria cause micolactone (a toxin) and they cause borrelia ulcers -inflammatory illness caused by compounds made by a living organism. If they were benign, we should not worry about them, but they do hurt us. Not everyone is able to clear these toxins. In our published data, about 22% of those who get Lyme disease has a genetic makeup that means that they will not be able to mount an effective clearing and healing response to the toxins. If they cannot be cleared (and they tend to stay because they move from cell to cell), they can create a chronic illness characterized by inflammation that antibiotics will not heal.
Sue: Is there such a thing as a"high-functioning" Lymie?
Dr. Shoemaker: One of the real issues that I look at is the diversity of responsive people to illnesses characterized by chronic inflammation. There are some people that I call Superman (or Superwoman). A simple example of this is a med student from Johns Hopkins that was training with me who thought that this patient couldn't possibly be one of my patients -- he runs 2 miles a day. I walk in and ask the patient if he ran before he got Lyme disease and he says that he did. I asked how far he ran before he got Lyme disease and he responds that he used to run 10 miles a day.
Sue: How did you become involved with Lyme disease and biotoxins?
Dr. Shoemaker: Borrelia (a biotoxin) was the turning point in my life. I started in 1997 with a little critter like an algae, and we saw how it created a multi-symptom illness that was treated successfully with cholestyramine, a drug that has been around for 50 years. When I gave this medication to my blue-green algae patients, they got better. When I gave it to my mold patients, they got better.
In 1999, when I heard that Dr. Sam Donta's group in Boston had presented data on the BB neurotoxin made by Borellia, I reasoned that cholestyramine would work on my Lyme patients. Well, they didn't get better - they got worse. It was that worsening that really greased the wheels - why was this happening; what was going on? It opened the door to cytokines and inflammation because we then learned that if we take steps before giving a post-Lyme patient, after they have been treated with antibiotics, cholestyramine first, if we gave them compounds that blocked the inflammatory cytotkine responses, we didn't get this horrible worsening.
It says that a large part of the chronic inflammation in the post-Lyme patients is cytokine mediated, and if we follow that train of thought, excessive cytokine responses do other things, too. They can participate in a variety of ways with damaging other elements in what is called the innate immune response - basically a group of different elements that preformed and are ready to go to fight off offending antigens, invaders, if you will, and cytokines are part of that. The overall controller of these innate immune responses is a hormone made in the brain called MSH (melanocyte-stimulating hormone). And this was all the information that got started with Lyme.
Sue: How can a person with Lyme tell if they have a biotoxin illness?
Dr. Shoemaker: One of the nice things, thanks to work done by a neurotoxicologist at the U.S.E.P.A. (United States Environmental Protection Agency) and the National Health and Environmental Effects Research Lab, particular deficits can be identified with a special test called Visual Contrast Sensitivity (VCS). It's a simple test - cover one eye, once we know your visual acuity (being able to see better than 20/50), and we look at this patented, published device, a card that has 5 different frequencies of stimuli (called bars), with 9 different patches for each of the five frequencies. Each bar, as we move from left to right, has a diminishing intensity of coloration (black bars on a gray background). The toxicology folks have known for 40 years how to use this test as it's used on fighter pilots to separate an enemy against the gray background.
Using this test has shown to be effective because it shows distinctive deficits in the ability to recognize these wave patterns in each of the five frequencies when used on biotoxin patients. So, if you have Lyme and you have antibiotics and you stay sick after antibiotics, the first thing I am going to do is a complete recording of the patient's symptoms and also a VCS (it takes five minutes, is noninvasive, inexpensive, and is reproducibly reliable).
Sue: Will this test tell you if your patient has a biotoxin illness?
Dr. Shoemaker: It will tell you with a very high degree of likelihood that the potential is there. Only 92% of our biotoxin patients have a positive test (they show the distinctive deficit). Fortunately, less than 1% of normal people show this deficit. So we have a pretty good track record on absence of false positives and relatively few false negatives. If all we needed to diagnose these patients were a VCS, well, quite frankly, we wouldn't need anything else.
Typically, the labs looking at abnormalities are using my protocol around the country and ordering profiling lab tests after we have the potential for exposure (i.e. you have Lyme), have multiple system involvement with multiple symptoms, and you have this deficit. If you are tired because you are depressed, chances are you won't have the visual contrast deficit (usually), but you certainly won't have the lab abnormalities. So it's focusing on sensitivity and specificity that helps bring the diagnosis home.
In so many people that I see, they come and are desperately wanting, in addition to feeling better, to have some validation that there is something wrong. With this test, it's one easy way that opens the door to look at mechanisms that could be going on to explain this deficit. That means that we can draw blood and we can put your illness on a piece of paper.
The exciting advances that the research community is making following this approach is that we now have ways of looking at folks who have cognitive disorders and brain fog; measuring with an MRI machine, we can measure a variety of particular, abnormal compounds in the brain with inflammatory markers in the blood that correlate with symptoms. Even better, when you fix the inflammatory markers in the blood, with targeted individual therapy, we watch symptoms disappear, but more importantly, watch the chemical basis for those things disappear. If the patient has another exposure to mold or a tick bite, and they get sick again, those same abnormalities come back coinciding with the symptoms. Seeing people get better is the most excitement in medicine I have ever had. Biotoxins have direct effects on nerve cells, making the VCS a necessary test for probability of the presence of a biotoxin.
Sue: What is C4a?
Dr. Shoemaker: One of the activation products of complement; one of the innate immune response elements that's hugely important as a marker, not just in mold and Lyme patients, but in other biotoxin patients as well. C4a will rise in 4 hours after mold exposure and 12 hours after a tick bite if someone is going to have Lyme disease (a good acute marker). The higher elevation of C4a stays up if:
1. You have living Lyme organisms
2. You have a biotoxin.
So what we do is follow C4a. C4a (RIA) is a lab test - Quest is the lab.
Sue: What is your work looking at now?
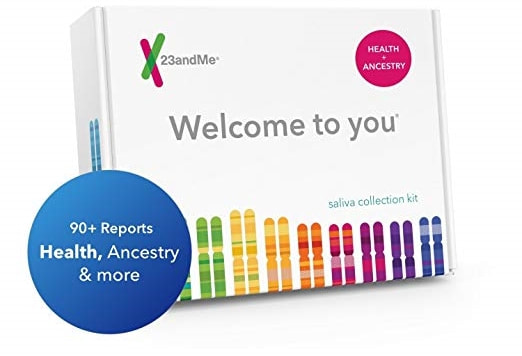
Dr. Shoemaker: Genomics. If we think that inflammation is part of the problem, then the gene’s coding for those inflammatory chemicals are ones that we should be able to identify and recognize as they become activated and as the illness develops - and we can do that.
Sue: What role do immune response genes have in thinking about post-Lyme syndrome?
Dr. Shoemaker: I think that we can target and profile what is wrong immunologically at the source of inflammation that results in a constellation of symptoms that get called "post-Lyme." The big deal to me is how can we sort out whether or not a patient has living Lyme organisms after they've been on antibiotics. I don't know who has the answer, but I do know that so far, our model is holding up.
Sue: What is histocompatibility locus A (HLA)?
Dr. Shoemaker: HLA controls immune response. HLA genes code various proteins on the outer portion of cells. The immune system uses HLA to determine the difference between "self" and "non-self". HLA is involved in the steps responsible for antibody formation. These genes have been associated with an inability of the body to recover from illnesses resulting from Lyme disease, molds, and other sources.
In the event that a person has a susceptible genotype, the body does not recognize the toxins as a foreign invader and thus, they are allowed to remain in the body. This causes long-term and perpetual ill-health. It has been asserted that nearly 100% of people that become ill after exposure to a biotoxin can be shown to have a predisposition to that biotoxin through the HLA-DR genotype. Many of us have bodies that simply do not recognize the presence of these toxic substances and thus do nothing to eliminate them.
"Dr. Shoemaker uses the terms "Lyme susceptible" or "mold susceptible" or "multi-susceptible" to categorize one's HLA genotype." (BetterHealthGuy.com)
Sue: Let's say that I have Lyme disease and no one questions the diagnosis. I have received the 21 days of Doxycycline and I am still sick. What now?
Dr. Shoemaker: We look at the 37 symptoms on the list (note that biotoxin symptoms are almost the same), but the symptoms won't tell you all you need to know. What needs to be done:
1. Make sure they don't have a compounding exposure (many folks with Lyme might be exposed to mold and not recognize that the mold is making them sick after the Lyme opens up the disease, and they say that they need more antibiotics - mold does not respond to antibiotics).
2. Rule out other diseases.
Sue: What if it's Lyme, and Lyme only? What is the gene signature - the HLA?
Dr. Shoemaker: If you have Lyme and HLA, you are not going to respond to antibiotics - they are going to have the biotoxin aspect.
Sue: Do most physicians know they should be looking at the C4a?
Dr. Shoemaker: Judging by the phone calls we get, we need to do a lot more education. The trouble is that if you don't have peer-reviewed research published, what you know to be true does not exist. One of the things I worry about with Lyme patients is that you won't know how your C4a or MSH is by how you feel. But if MSH is low, and you don't have the normal control of inflammatory responses, and say you walk into a moldy building and get slammed, the C4a response doesn't just go up to the level as it was before, it goes up exceptionally high. And I use the expression "sicker, quicker" as my shorthand same as saying, "Look out!"
Sue: I've done the VCS and the lab work for the biotoxin pathway - now what?
Dr. Shoemaker: Actos is what I use for my Lyme patients (45 mg taken with my special diet that avoids foods that makes blood sugar go up quickly - amylose). Actos is not given to "people who are real skinny," as Actos will make them feel "bad."
Sue: Actos has been given a "black box" warning from the federal Food and Drug Administration (FDA). Is it safe to use off label?
Dr. Shoemaker: Actos has been around for about 10 years and I have used it in over 6,000 patients. With the no amylose diet and Actos taken short term, we've seen no significant adverse effects from liver abnormalities or heart problems at all. I am not afraid of Actos at all. But I do make sure that people who are taking it are informed that it is a potential concern to the FDA.
Sue: What is the amylose diet?
Dr. Shoemaker: It's a diet that focuses on eating fresh fruits, fresh vegetables and plenty of protein. Keep away from vegetables that grow below the ground (peanuts and potatoes), garlic and onions are okay, but no wheat, rice, oats, barley and rye, and also no bananas.
Sue: What is a biotoxin?
Dr. Shoemaker: Living organisms produce biotoxins. These biotoxins are small compounds made by living creatures. However, neurotoxins go from cell to cell and bind to particular types of receptors. Once done, a biological effect is started. One toxin will set off ten inflammatory cascades or results and that ten each sets off ten more, and soon - all very rapidly.
Sue: What is a microbacteria?
Dr. Shoemaker: Tuberculosis is one kind of a microbacteria. The importance of this is that microbacteria cause micolactone (a toxin) and they cause borrelia ulcers -inflammatory illness caused by compounds made by a living organism. If they were benign, we should not worry about them, but they do hurt us. Not everyone is able to clear these toxins. In our published data, about 22% of those who get Lyme disease has a genetic makeup that means that they will not be able to mount an effective clearing and healing response to the toxins. If they cannot be cleared (and they tend to stay because they move from cell to cell), they can create a chronic illness characterized by inflammation that antibiotics will not heal.
Sue: Is there such a thing as a"high-functioning" Lymie?
Dr. Shoemaker: One of the real issues that I look at is the diversity of responsive people to illnesses characterized by chronic inflammation. There are some people that I call Superman (or Superwoman). A simple example of this is a med student from Johns Hopkins that was training with me who thought that this patient couldn't possibly be one of my patients -- he runs 2 miles a day. I walk in and ask the patient if he ran before he got Lyme disease and he says that he did. I asked how far he ran before he got Lyme disease and he responds that he used to run 10 miles a day.
Sue: How did you become involved with Lyme disease and biotoxins?
Dr. Shoemaker: Borrelia (a biotoxin) was the turning point in my life. I started in 1997 with a little critter like an algae, and we saw how it created a multi-symptom illness that was treated successfully with cholestyramine, a drug that has been around for 50 years. When I gave this medication to my blue-green algae patients, they got better. When I gave it to my mold patients, they got better.
In 1999, when I heard that Dr. Sam Donta's group in Boston had presented data on the BB neurotoxin made by Borellia, I reasoned that cholestyramine would work on my Lyme patients. Well, they didn't get better - they got worse. It was that worsening that really greased the wheels - why was this happening; what was going on? It opened the door to cytokines and inflammation because we then learned that if we take steps before giving a post-Lyme patient, after they have been treated with antibiotics, cholestyramine first, if we gave them compounds that blocked the inflammatory cytotkine responses, we didn't get this horrible worsening.
It says that a large part of the chronic inflammation in the post-Lyme patients is cytokine mediated, and if we follow that train of thought, excessive cytokine responses do other things, too. They can participate in a variety of ways with damaging other elements in what is called the innate immune response - basically a group of different elements that preformed and are ready to go to fight off offending antigens, invaders, if you will, and cytokines are part of that. The overall controller of these innate immune responses is a hormone made in the brain called MSH (melanocyte-stimulating hormone). And this was all the information that got started with Lyme.
Sue: How can a person with Lyme tell if they have a biotoxin illness?
Dr. Shoemaker: One of the nice things, thanks to work done by a neurotoxicologist at the U.S.E.P.A. (United States Environmental Protection Agency) and the National Health and Environmental Effects Research Lab, particular deficits can be identified with a special test called Visual Contrast Sensitivity (VCS). It's a simple test - cover one eye, once we know your visual acuity (being able to see better than 20/50), and we look at this patented, published device, a card that has 5 different frequencies of stimuli (called bars), with 9 different patches for each of the five frequencies. Each bar, as we move from left to right, has a diminishing intensity of coloration (black bars on a gray background). The toxicology folks have known for 40 years how to use this test as it's used on fighter pilots to separate an enemy against the gray background.
Using this test has shown to be effective because it shows distinctive deficits in the ability to recognize these wave patterns in each of the five frequencies when used on biotoxin patients. So, if you have Lyme and you have antibiotics and you stay sick after antibiotics, the first thing I am going to do is a complete recording of the patient's symptoms and also a VCS (it takes five minutes, is noninvasive, inexpensive, and is reproducibly reliable).
Sue: Will this test tell you if your patient has a biotoxin illness?
Dr. Shoemaker: It will tell you with a very high degree of likelihood that the potential is there. Only 92% of our biotoxin patients have a positive test (they show the distinctive deficit). Fortunately, less than 1% of normal people show this deficit. So we have a pretty good track record on absence of false positives and relatively few false negatives. If all we needed to diagnose these patients were a VCS, well, quite frankly, we wouldn't need anything else.
Typically, the labs looking at abnormalities are using my protocol around the country and ordering profiling lab tests after we have the potential for exposure (i.e. you have Lyme), have multiple system involvement with multiple symptoms, and you have this deficit. If you are tired because you are depressed, chances are you won't have the visual contrast deficit (usually), but you certainly won't have the lab abnormalities. So it's focusing on sensitivity and specificity that helps bring the diagnosis home.
In so many people that I see, they come and are desperately wanting, in addition to feeling better, to have some validation that there is something wrong. With this test, it's one easy way that opens the door to look at mechanisms that could be going on to explain this deficit. That means that we can draw blood and we can put your illness on a piece of paper.
The exciting advances that the research community is making following this approach is that we now have ways of looking at folks who have cognitive disorders and brain fog; measuring with an MRI machine, we can measure a variety of particular, abnormal compounds in the brain with inflammatory markers in the blood that correlate with symptoms. Even better, when you fix the inflammatory markers in the blood, with targeted individual therapy, we watch symptoms disappear, but more importantly, watch the chemical basis for those things disappear. If the patient has another exposure to mold or a tick bite, and they get sick again, those same abnormalities come back coinciding with the symptoms. Seeing people get better is the most excitement in medicine I have ever had. Biotoxins have direct effects on nerve cells, making the VCS a necessary test for probability of the presence of a biotoxin.
Sue: What is C4a?
Dr. Shoemaker: One of the activation products of complement; one of the innate immune response elements that's hugely important as a marker, not just in mold and Lyme patients, but in other biotoxin patients as well. C4a will rise in 4 hours after mold exposure and 12 hours after a tick bite if someone is going to have Lyme disease (a good acute marker). The higher elevation of C4a stays up if:
1. You have living Lyme organisms
2. You have a biotoxin.
So what we do is follow C4a. C4a (RIA) is a lab test - Quest is the lab.
Sue: What is your work looking at now?
Dr. Shoemaker: Genomics. If we think that inflammation is part of the problem, then the gene’s coding for those inflammatory chemicals are ones that we should be able to identify and recognize as they become activated and as the illness develops - and we can do that.
Sue: What role do immune response genes have in thinking about post-Lyme syndrome?
Dr. Shoemaker: I think that we can target and profile what is wrong immunologically at the source of inflammation that results in a constellation of symptoms that get called "post-Lyme." The big deal to me is how can we sort out whether or not a patient has living Lyme organisms after they've been on antibiotics. I don't know who has the answer, but I do know that so far, our model is holding up.
Sue: What is histocompatibility locus A (HLA)?
Dr. Shoemaker: HLA controls immune response. HLA genes code various proteins on the outer portion of cells. The immune system uses HLA to determine the difference between "self" and "non-self". HLA is involved in the steps responsible for antibody formation. These genes have been associated with an inability of the body to recover from illnesses resulting from Lyme disease, molds, and other sources.
In the event that a person has a susceptible genotype, the body does not recognize the toxins as a foreign invader and thus, they are allowed to remain in the body. This causes long-term and perpetual ill-health. It has been asserted that nearly 100% of people that become ill after exposure to a biotoxin can be shown to have a predisposition to that biotoxin through the HLA-DR genotype. Many of us have bodies that simply do not recognize the presence of these toxic substances and thus do nothing to eliminate them.
"Dr. Shoemaker uses the terms "Lyme susceptible" or "mold susceptible" or "multi-susceptible" to categorize one's HLA genotype." (BetterHealthGuy.com)
Sue: Let's say that I have Lyme disease and no one questions the diagnosis. I have received the 21 days of Doxycycline and I am still sick. What now?
Dr. Shoemaker: We look at the 37 symptoms on the list (note that biotoxin symptoms are almost the same), but the symptoms won't tell you all you need to know. What needs to be done:
1. Make sure they don't have a compounding exposure (many folks with Lyme might be exposed to mold and not recognize that the mold is making them sick after the Lyme opens up the disease, and they say that they need more antibiotics - mold does not respond to antibiotics).
2. Rule out other diseases.
Sue: What if it's Lyme, and Lyme only? What is the gene signature - the HLA?
Dr. Shoemaker: If you have Lyme and HLA, you are not going to respond to antibiotics - they are going to have the biotoxin aspect.
Sue: Do most physicians know they should be looking at the C4a?
Dr. Shoemaker: Judging by the phone calls we get, we need to do a lot more education. The trouble is that if you don't have peer-reviewed research published, what you know to be true does not exist. One of the things I worry about with Lyme patients is that you won't know how your C4a or MSH is by how you feel. But if MSH is low, and you don't have the normal control of inflammatory responses, and say you walk into a moldy building and get slammed, the C4a response doesn't just go up to the level as it was before, it goes up exceptionally high. And I use the expression "sicker, quicker" as my shorthand same as saying, "Look out!"
Sue: I've done the VCS and the lab work for the biotoxin pathway - now what?
Dr. Shoemaker: Actos is what I use for my Lyme patients (45 mg taken with my special diet that avoids foods that makes blood sugar go up quickly - amylose). Actos is not given to "people who are real skinny," as Actos will make them feel "bad."
Sue: Actos has been given a "black box" warning from the federal Food and Drug Administration (FDA). Is it safe to use off label?
Dr. Shoemaker: Actos has been around for about 10 years and I have used it in over 6,000 patients. With the no amylose diet and Actos taken short term, we've seen no significant adverse effects from liver abnormalities or heart problems at all. I am not afraid of Actos at all. But I do make sure that people who are taking it are informed that it is a potential concern to the FDA.
Sue: What is the amylose diet?
Dr. Shoemaker: It's a diet that focuses on eating fresh fruits, fresh vegetables and plenty of protein. Keep away from vegetables that grow below the ground (peanuts and potatoes), garlic and onions are okay, but no wheat, rice, oats, barley and rye, and also no bananas.
About the author
Ritchie C. Shoemaker graduated medical school from Duke University (1969-1973) Magna Cum Laude. He is the President of Chronic Neurotoxins, Inc.; Medical Director at the Center for Research on Biotoxin Associated Illnesses; and has a private practice in Pocomoke, Maryland. Dr. Shoemaker has appeared on numerous television and radio shows, received many awards, and has a long list of publications. His website is moldwarriors.com and he was a guest on In Short Order radio show with Sue Vogan (highway2health.net) on October 4, 2007. His new book, "Surviving Mold," is due out in the spring of 2008 - available at moldwarriors.com and Amazon.
latest posts
tags
Disclaimer: The information on this website is not a substitute for professional medical advice.
Always consult with your treating physician before altering any treatment protocol.
Always consult with your treating physician before altering any treatment protocol.