NeuroImmunology: From Leaky Gut to Leaky Brain
December 1, 2008 in science & Research by Scott Forsgren
Many people with chronic Lyme disease understand what it means to have ongoing digestive complaints, brain fog, cognitive deficits, joint pain, and more. However, the connections between the digestive system, the immune system, and the nervous systems of the body are often overlooked.
Aristo Vojdani, PhD, is a research scientist and immunologist in the emerging field of NeuroImmunology. Dr. Vojdani is the head of Immunosciences Lab, Inc. and works closely with researchers at Neuroscience, Inc. to create innovative laboratory solutions for patients and doctors wishing to explore these connections.
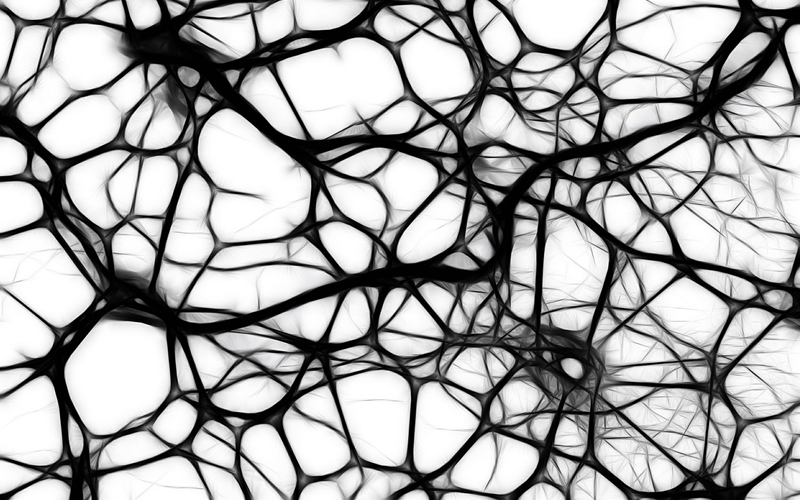
NeuroImmunology is the integration of neurology and immunology in clinical practice. Elaborate interactions exist in the body between the immune system and the nervous system, and these interactions have powerful effects on our overall health. The field of NeuroImmunology will be the guide for many years to come as patients and doctors work to solve complex neuroimmune diseases.
Lyme disease is classified as a neuroimmune disorder, as are Lupus, Celiac disease, autism, and many others. Neuroimmune disorders are complex disease processes that are induced by three main environmental factors:
The contribution of infections and toxicity to poor health has been known for some time. However, the focus on dietary proteins and peptides and how these affect the immune system, the nervous system, and even how they contribute to autoimmune disease and neurodegenerative conditions is not often discussed.
Due to the similarities of dietary proteins and peptides to human tissues, the body may create antibodies to items consumed in our diet which then, as a result of cross-reactivity with our own tissues, attack our bodies and lead to autoimmune and neuroimmune disorders. A classic example is the connection between milk and diabetes, or between gluten and cerebellar ataxia.
Neuroimmune disorders often start in the gastrointestinal tract which may then affect the immune system and later manifest in the nervous system. The end result of these disorders is a direct and powerful negative impact on brain function which leads to a myriad of symptoms.
Looking at the factors that lead to neuroimmune disorders in more detail, a number of potential contributors are known:
It does not take long for one to recognize that there are many factors which lead the body to a state of Leaky Gut Syndrome. Once a leaky gut is present, the downstream effects can be disastrous. It literally does go "From Leaky Gut to Leaky Brain" as we will soon see.
All of the contributors to neuroimmune disorders listed above induce mucosal immune dysregulation which results in the production of pro-inflammatory cytokines such as IL-1β. These cytokines, or signaling proteins which regulate cellular communication in the body, then bind to receptors very near to what are known as "tight junction complexes".
Tight junction complexes are important in ensuring mucosal integrity which is a key to maintaining a healthy digestive tract. A healthy digestive tract is one which does not allow dietary proteins and peptides into the bloodstream.
Next, a cascade is initiated which activates NF-kb, a protein involved in our ability to respond to stress, cytokines, free radicals, and infections. NF-kb also plays an important role in regulating the immune system's response to infection.
This activation further leads to the breakdown of these tight junctions and then creates openings in the digestive tract through which unexpected molecules can easily pass into the blood and systemic circulation. Once this occurs, we have what is commonly known as "Leaky Gut Syndrome".
For those with Leaky Gut Syndrome, particles of food cross through the lining of the digestive tract and into systemic circulation. Once in circulation, the body's immune system organizes an attack on these foreign objects through the production of antibodies.
Once these barriers are broken, food intolerances and sensitivities develop. If this leaky gut condition is not addressed, the end result is autoimmunity and, in many cases, "leaky brain".
The body has four major barriers intended to protect itself from substances that should not be present in us. These are:
The two most important in the world of NeuroImmunology are the intestinal barrier and the blood-brain barrier. In the past, autoimmune conditions have been blamed on genetics and environmental factors. However, recent studies suggest that there is a third element involved which is the loss of intestinal barrier function.
If intestinal barrier dysfunction, commonly referred to as Leaky Gut Syndrome, can be corrected, one can often succeed in addressing autoimmunity. Any attempt to treat an autoimmune disorder without special attention to intestinal barrier function will likely result in less than optimal patient outcomes.
Mucosal immunity, the immune system found in the mucous membranes of the body, is our first line of defense. It must properly respond to bacteria, viruses, dietary proteins and peptides, and numerous other substances.
Secretory IgA testing is the primary laboratory tool that can be used to evaluate mucosal immunity. If SIgA is low, this potentially suggests autoimmunity. If SIgA is high, the possibility of infection in either the oral cavity or gastrointestinal tract is present. Both high and low SIgA contribute to intestinal barrier dysfunction. IgA plays an important role in responding to dietary antigens and microbes that are ingested and prevents their passage into systemic circulation.
A small percentage of the population is IgA deficient which could lead to false negative results. Thus, the preferred approach to testing for various dietary proteins and peptides is to include both IgA and IgM antibodies first and then IgG later.
Dr. Vojdani has developed Intestinal Barrier Function testing to evaluate for the presence of Leaky Gut Syndrome. The majority of tests today which evaluate intestinal barrier function use lactulose or mannitol as the molecule which indicates whether or not the gut is in fact leaky.
Lactulose and mannitol are very small molecules. Dr. Vojdani suggests that if we look at a fly versus an elephant, the body may not respond to a fly but will respond to an elephant. Thus, Dr. Vojdani's tests use large molecules which are more likely to provoke immune responses due to the antigenic nature of these larger molecules. It is Dr. Vojdani's opinion that testing for intestinal barrier dysfunction with lactulose or mannitol could result in false positive test results.
The body is exposed to many dietary proteins and peptides on a daily basis. Wheat, corn, soy, milk, and egg are common dietary proteins which are included in the Intestinal Barrier Function test.
The test further includes Candida species, aerobic bacteria such as E. coli and Enterococcus, and anaerobic bacteria such as Bacteroides fragilis and Clostridium perfringens.
When these antigens get into the blood, antibodies are created. If IgM antibodies are found to these common dietary proteins and various organisms, then the patient has Leaky Gut Syndrome to large antigenic molecules.
Now that the first line of defense, mucosal immunity, has been evaluated, the second line of defense is systemic immunity. Here, testing evaluates both immediate hypersensitivities and delayed hypersensitivities. Immediate hypersensitivities to dietary proteins and peptides are evaluated with IgE antibodies while delayed hypersensitivities are evaluated with IgG and IgA antibodies. These tests are performed using serum.
Contributors to inflammation in the gut include gluteomorphins (from gluten), casomorpins (from casein found in dairy products), and lectins (toxic compounds found in grains, dairy, nightshades, and legumes).
Given that a significant amount of the inflammation in the digestive tract can be attributed to foods that we consume, evaluation of intolerances and sensitivities and avoidance of offending substances cannot be overemphasized.
Most food allergy testing performed today uses raw foods such as meat, beans, or potatoes. Dr. Vojdani recognized that very few people eat raw foods. The same foods when cooked often cause significant reactions. The idea was carried further through the creation of a patent-pending test which evaluates for sensitivities to French fries, donuts, cake, Buffalo wings, and many more regularly consumed food products which are commonly part of the American diet.
Antibodies against dietary proteins and peptides contribute significantly to poor health through induction of imbalanced gut flora and release of endotoxins such as lipopolysaccharides (LPS). This was evidenced by a study in which LPS, an endotoxin which induces a response from any healthy immune system, were introduced to epithelial cells.
Introduction of LPS led to the production of pro-inflammatory cytokines as would be expected of a functional immune system. The researchers then took antibodies from a patient with Celiac disease and added them to the same cells. The result was a similarly high level of proinflammatory cytokine production.
After having been on a gluten free diet for six months, the same test was repeated and no pro-inflammatory cytokines were produced. This shows that gluten-free diets work and may be an important part of recovery for those suffering from neuroimmune disorders, including from Lyme disease, if the outcome is the elimination from the system of the agent responsible for neuroinflammation.
Dr. Vojdani has suggested that gliadin (a protein found in wheat) cross-reacts with peptides in the cerebellum, the portion of the brain responsible for sensory perception, coordination, and motor control.
When a patient makes antibodies against wheat, for example, and these antibodies then encounter cerebellum tissue, there is a significant cross-reaction and these antibodies therefore attack our own brains.
Gluten sensitivity is a complex issue which has now been shown to have significant impacts to the immune system and the nervous system, including the brain.
Food sensitivities and Leaky Gut Syndrome lead to systemic inflammation. Once the entire body reacts and enters a state of inflammatory response, a multitude of additional symptoms may be observed. Major depressive disorders, for example, have been linked to pro-inflammatory cytokines which result from a dysfunctional intestinal barrier.
Looking further at inflammation within the body, inflammation due to pro-inflammatory cytokines attracts molecules which have receptors on the blood-brain barrier.
Slowly, these molecules end up in the brain compartment and cause destruction of nerve cells. This entire process starts in the gut and results in a neuroimmune disorder including autoimmunity to the brain.
Similarly, in looking at the blood-brain barrier, large molecules are generally not permitted access to the brain. However, under conditions such as stress, toxic chemical exposures, and other conditions, the blood-brain barrier becomes more permeable.
There are three types of cells in the nervous system: astrocytes, neurons, and microglia. Each of these can become targets of neuroautoimmunity. Antibodies can be measured to each of these types of cells to evaluate for the presence of neuro-autoimmunity.
To evaluate the connection between the gut and the brain, two main tests can be ordered. As Dr. Vojdani suggests, "From leaky gut to leaky brain, the Intestinal Barrier Function and Blood-Brain Barrier (BBB) antibody tests are the most important places to begin."
Dr. Vojdani offers the "NeuroImmunology of Lyme, Panel C" which includes not only a series of tests for Lyme disease and co-infections, but also specifically looks at antibodies produced to the bloodbrain barrier which is an indicator of neuro-autoimmunity.
Several other antibodies can be evaluated for neuroimmunological conditions such as Myelin Basic Protein, Myelin Oligodendrocyte Glycoprotein, Myelin Associated Glycoprotein, Alpha-BCrystallin, Proteolipid Protein, Gliadin, Gluteomorphins, Casomorphins, Cerebellar tissue, and more. These antibodies can serve as good markers to track the effectiveness of treatment in quelling autoimmune conditions.
A clear connection has been drawn between the health of the gut and the health of the brain. A leaky gut allows for molecules to pass into systemic circulation which then activate an inflammatory response and the resulting pro-inflammatory cytokines can induce a host of autoimmune and neuroimmune disorders.
Evaluation of Intestinal Barrier Function and Blood-Brain Barrier protein antibodies are two important tools in identifying these presence of these conditions and defining a treatment plan that provides the patient with the best possible outcome. Here's to your health.
Aristo Vojdani, PhD, is a research scientist and immunologist in the emerging field of NeuroImmunology. Dr. Vojdani is the head of Immunosciences Lab, Inc. and works closely with researchers at Neuroscience, Inc. to create innovative laboratory solutions for patients and doctors wishing to explore these connections.
NeuroImmunology is the integration of neurology and immunology in clinical practice. Elaborate interactions exist in the body between the immune system and the nervous system, and these interactions have powerful effects on our overall health. The field of NeuroImmunology will be the guide for many years to come as patients and doctors work to solve complex neuroimmune diseases.
Lyme disease is classified as a neuroimmune disorder, as are Lupus, Celiac disease, autism, and many others. Neuroimmune disorders are complex disease processes that are induced by three main environmental factors:
- Infections
- Toxic chemicals
- Dietary proteins and peptides
The contribution of infections and toxicity to poor health has been known for some time. However, the focus on dietary proteins and peptides and how these affect the immune system, the nervous system, and even how they contribute to autoimmune disease and neurodegenerative conditions is not often discussed.
Due to the similarities of dietary proteins and peptides to human tissues, the body may create antibodies to items consumed in our diet which then, as a result of cross-reactivity with our own tissues, attack our bodies and lead to autoimmune and neuroimmune disorders. A classic example is the connection between milk and diabetes, or between gluten and cerebellar ataxia.
Neuroimmune disorders often start in the gastrointestinal tract which may then affect the immune system and later manifest in the nervous system. The end result of these disorders is a direct and powerful negative impact on brain function which leads to a myriad of symptoms.
Looking at the factors that lead to neuroimmune disorders in more detail, a number of potential contributors are known:
- Stress can render the blood-brain barrier (BBB) permeable and leave it in an "open" state whereby toxins and infections that should not be allowed entry into the brain are provided easy access through this dysfunctional barrier. Gulf-War Syndrome is a prime example. Stress negatively impacts both the immune system and the nervous system.
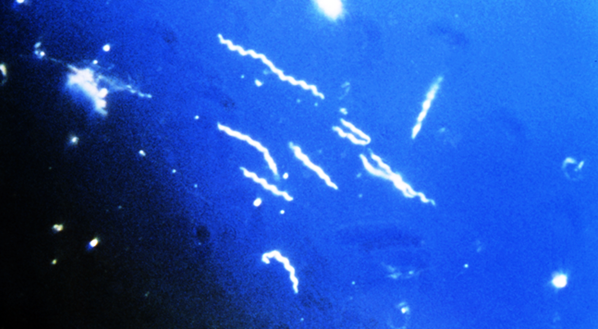
- Infections such as streptococcus, PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections, which in adults is simply known as ANDAS), and others.
- Dysfunctional enzymes can lead to Leaky Gut Syndrome which has significant implications for the immune system and nervous system.
- Xenobiotics are chemicals that are found in the environment but are not normally expected to be present in the human body The most common types of xenobiotics include pollutants such as dioxins and PCBs. One in particular that has recently gained notoriety is Bisphenol A (BPA), a material used in the manufacturing of plastics. BPA has now been detected in the urine of 95% of Americans tested. An interesting point to note for those of us with Lyme disease is that antibiotics themselves are considered xenobiotics and thus may contribute to neuroimmune disorders.
- Dietary proteins and peptides are found in the foods we consume and when Leaky Gut Syndrome is present, a cascade is initiated which results in neuroimmune disorders.
- Advanced Glycation End products (AGEs) are the end products of a reaction between sugars and proteins and result in compounds which have many negative health implications. Though AGEs can be created inside the body, they most often originate from outside the body through the heating of sugars with fats or proteins. A significant contributor to AGE body burden is found in high-fat, high-protein foods that are fried. For those with neuroimmune disorders, fried foods should generally be avoided entirely.
- Neurotransmitter (NT) abnormalities are implicated in Leaky Gut Syndrome.
It does not take long for one to recognize that there are many factors which lead the body to a state of Leaky Gut Syndrome. Once a leaky gut is present, the downstream effects can be disastrous. It literally does go "From Leaky Gut to Leaky Brain" as we will soon see.
All of the contributors to neuroimmune disorders listed above induce mucosal immune dysregulation which results in the production of pro-inflammatory cytokines such as IL-1β. These cytokines, or signaling proteins which regulate cellular communication in the body, then bind to receptors very near to what are known as "tight junction complexes".
Tight junction complexes are important in ensuring mucosal integrity which is a key to maintaining a healthy digestive tract. A healthy digestive tract is one which does not allow dietary proteins and peptides into the bloodstream.
Next, a cascade is initiated which activates NF-kb, a protein involved in our ability to respond to stress, cytokines, free radicals, and infections. NF-kb also plays an important role in regulating the immune system's response to infection.
This activation further leads to the breakdown of these tight junctions and then creates openings in the digestive tract through which unexpected molecules can easily pass into the blood and systemic circulation. Once this occurs, we have what is commonly known as "Leaky Gut Syndrome".
For those with Leaky Gut Syndrome, particles of food cross through the lining of the digestive tract and into systemic circulation. Once in circulation, the body's immune system organizes an attack on these foreign objects through the production of antibodies.
Once these barriers are broken, food intolerances and sensitivities develop. If this leaky gut condition is not addressed, the end result is autoimmunity and, in many cases, "leaky brain".
The body has four major barriers intended to protect itself from substances that should not be present in us. These are:
- Skin barrier
- Lung barrier
- Intestinal barrier
- Blood-brain barrier
The two most important in the world of NeuroImmunology are the intestinal barrier and the blood-brain barrier. In the past, autoimmune conditions have been blamed on genetics and environmental factors. However, recent studies suggest that there is a third element involved which is the loss of intestinal barrier function.
If intestinal barrier dysfunction, commonly referred to as Leaky Gut Syndrome, can be corrected, one can often succeed in addressing autoimmunity. Any attempt to treat an autoimmune disorder without special attention to intestinal barrier function will likely result in less than optimal patient outcomes.
Mucosal immunity, the immune system found in the mucous membranes of the body, is our first line of defense. It must properly respond to bacteria, viruses, dietary proteins and peptides, and numerous other substances.
Secretory IgA testing is the primary laboratory tool that can be used to evaluate mucosal immunity. If SIgA is low, this potentially suggests autoimmunity. If SIgA is high, the possibility of infection in either the oral cavity or gastrointestinal tract is present. Both high and low SIgA contribute to intestinal barrier dysfunction. IgA plays an important role in responding to dietary antigens and microbes that are ingested and prevents their passage into systemic circulation.
A small percentage of the population is IgA deficient which could lead to false negative results. Thus, the preferred approach to testing for various dietary proteins and peptides is to include both IgA and IgM antibodies first and then IgG later.
Dr. Vojdani has developed Intestinal Barrier Function testing to evaluate for the presence of Leaky Gut Syndrome. The majority of tests today which evaluate intestinal barrier function use lactulose or mannitol as the molecule which indicates whether or not the gut is in fact leaky.
Lactulose and mannitol are very small molecules. Dr. Vojdani suggests that if we look at a fly versus an elephant, the body may not respond to a fly but will respond to an elephant. Thus, Dr. Vojdani's tests use large molecules which are more likely to provoke immune responses due to the antigenic nature of these larger molecules. It is Dr. Vojdani's opinion that testing for intestinal barrier dysfunction with lactulose or mannitol could result in false positive test results.
The body is exposed to many dietary proteins and peptides on a daily basis. Wheat, corn, soy, milk, and egg are common dietary proteins which are included in the Intestinal Barrier Function test.
The test further includes Candida species, aerobic bacteria such as E. coli and Enterococcus, and anaerobic bacteria such as Bacteroides fragilis and Clostridium perfringens.
When these antigens get into the blood, antibodies are created. If IgM antibodies are found to these common dietary proteins and various organisms, then the patient has Leaky Gut Syndrome to large antigenic molecules.
Now that the first line of defense, mucosal immunity, has been evaluated, the second line of defense is systemic immunity. Here, testing evaluates both immediate hypersensitivities and delayed hypersensitivities. Immediate hypersensitivities to dietary proteins and peptides are evaluated with IgE antibodies while delayed hypersensitivities are evaluated with IgG and IgA antibodies. These tests are performed using serum.
Contributors to inflammation in the gut include gluteomorphins (from gluten), casomorpins (from casein found in dairy products), and lectins (toxic compounds found in grains, dairy, nightshades, and legumes).
Given that a significant amount of the inflammation in the digestive tract can be attributed to foods that we consume, evaluation of intolerances and sensitivities and avoidance of offending substances cannot be overemphasized.
Most food allergy testing performed today uses raw foods such as meat, beans, or potatoes. Dr. Vojdani recognized that very few people eat raw foods. The same foods when cooked often cause significant reactions. The idea was carried further through the creation of a patent-pending test which evaluates for sensitivities to French fries, donuts, cake, Buffalo wings, and many more regularly consumed food products which are commonly part of the American diet.
Antibodies against dietary proteins and peptides contribute significantly to poor health through induction of imbalanced gut flora and release of endotoxins such as lipopolysaccharides (LPS). This was evidenced by a study in which LPS, an endotoxin which induces a response from any healthy immune system, were introduced to epithelial cells.
Introduction of LPS led to the production of pro-inflammatory cytokines as would be expected of a functional immune system. The researchers then took antibodies from a patient with Celiac disease and added them to the same cells. The result was a similarly high level of proinflammatory cytokine production.
After having been on a gluten free diet for six months, the same test was repeated and no pro-inflammatory cytokines were produced. This shows that gluten-free diets work and may be an important part of recovery for those suffering from neuroimmune disorders, including from Lyme disease, if the outcome is the elimination from the system of the agent responsible for neuroinflammation.
Dr. Vojdani has suggested that gliadin (a protein found in wheat) cross-reacts with peptides in the cerebellum, the portion of the brain responsible for sensory perception, coordination, and motor control.
When a patient makes antibodies against wheat, for example, and these antibodies then encounter cerebellum tissue, there is a significant cross-reaction and these antibodies therefore attack our own brains.
Gluten sensitivity is a complex issue which has now been shown to have significant impacts to the immune system and the nervous system, including the brain.
Food sensitivities and Leaky Gut Syndrome lead to systemic inflammation. Once the entire body reacts and enters a state of inflammatory response, a multitude of additional symptoms may be observed. Major depressive disorders, for example, have been linked to pro-inflammatory cytokines which result from a dysfunctional intestinal barrier.
Looking further at inflammation within the body, inflammation due to pro-inflammatory cytokines attracts molecules which have receptors on the blood-brain barrier.
Slowly, these molecules end up in the brain compartment and cause destruction of nerve cells. This entire process starts in the gut and results in a neuroimmune disorder including autoimmunity to the brain.
Similarly, in looking at the blood-brain barrier, large molecules are generally not permitted access to the brain. However, under conditions such as stress, toxic chemical exposures, and other conditions, the blood-brain barrier becomes more permeable.
There are three types of cells in the nervous system: astrocytes, neurons, and microglia. Each of these can become targets of neuroautoimmunity. Antibodies can be measured to each of these types of cells to evaluate for the presence of neuro-autoimmunity.
To evaluate the connection between the gut and the brain, two main tests can be ordered. As Dr. Vojdani suggests, "From leaky gut to leaky brain, the Intestinal Barrier Function and Blood-Brain Barrier (BBB) antibody tests are the most important places to begin."
Dr. Vojdani offers the "NeuroImmunology of Lyme, Panel C" which includes not only a series of tests for Lyme disease and co-infections, but also specifically looks at antibodies produced to the bloodbrain barrier which is an indicator of neuro-autoimmunity.
Several other antibodies can be evaluated for neuroimmunological conditions such as Myelin Basic Protein, Myelin Oligodendrocyte Glycoprotein, Myelin Associated Glycoprotein, Alpha-BCrystallin, Proteolipid Protein, Gliadin, Gluteomorphins, Casomorphins, Cerebellar tissue, and more. These antibodies can serve as good markers to track the effectiveness of treatment in quelling autoimmune conditions.
A clear connection has been drawn between the health of the gut and the health of the brain. A leaky gut allows for molecules to pass into systemic circulation which then activate an inflammatory response and the resulting pro-inflammatory cytokines can induce a host of autoimmune and neuroimmune disorders.
Evaluation of Intestinal Barrier Function and Blood-Brain Barrier protein antibodies are two important tools in identifying these presence of these conditions and defining a treatment plan that provides the patient with the best possible outcome. Here's to your health.
About the author
Scott Forsgren (Author) is a health writer, advocate, and coach. He is the editor and founder of BetterHealthGuy.com where he shares his now 17 year journey through the world of Lyme disease and the myriad of factors that it often entails. He has been fortunate to have written for publications such as the Public Health Alert, Explore!, Bolen Report, and Townsend Letter. More information on his work is available at BetterHealthGuy.com.
latest posts
tags
Disclaimer: The information on this website is not a substitute for professional medical advice.
Always consult with your treating physician before altering any treatment protocol.
Always consult with your treating physician before altering any treatment protocol.