Microbes And Mental Illness
January 8, 2015 in Science/Research by Dr. Robert C. Bransfield, MD
Microbes are the greatest predator of man. As medical technology improves, there is increasing recognition that infectious disease contributes not only to acute, but also chronic relapsing illness and mental illness. The evidence to support this is a combination of insights from theoretical biology (particularly Darwinian medicine), research, and direct clinical observations.
We lead our entire lives surrounded by microbes. In a state of health, there is a balance, a reasonable resistance to infectious disease, and a peaceful co-existence. In contrast, with infectious disease, there is an imbalance between the threat posed by microbes and host defenses. This balance is affected by environmental factors (including exposure to pathogens) and a number of host factors such as genetics and/or increased vulnerability as a result of a state of chronic stress. Although the stress response is adaptive in a short time frame to allocate resources during a crisis, if the stress response is persistent, rather than cyclic, it further increases vulnerability to disease.
The most common sequence of disease begins with a vulnerability and an exposure to one or more stressors. The vulnerability may commonly include genetic and/or increased vulnerability as a result of chronic stress. As a result of these and other vulnerabilities, the microbe more easily penetrates the host's defenses and an initial infection may then occur.
Although infection may occur from microbes that are always present in the environment, a greater number of organisms or more virulent organisms further increase risk. Acute infections are most noteworthy in general medicine. However, the course of the infection most relevant to psychiatry includes injury from a prior infection; chronic, low-grade, persistent relapsing infections; or the persistence of the infectious agent in the inactive state. When persistent, relapsing infection occurs, there may be extended period of latency followed by some triggering event(s) (i.e.: chronic stress, injury, surgery, or other infectious agents), which may then cause the activation of the infectious agent(s) and the progression of the pathological process.
Some injury in infectious disease is a result of toxic products or direct cell injury, but a significant amount of injury is a result of host defenses gone awry in response to the infection. Neural injury may occur by a variety of mechanisms, which include vasculitis, direct cell injury, toxins, inflammation, cytokines, autoimmune mechanisms, incorporation of parasite DNA into host DNA, and excitotoxicity. This injury leads to a vicious cycle of disease, resulting in dysfunction of associative and/or modulating centers of the brain. Injury to associative centers more commonly causes cognitive symptoms, while injury to modulating centers more commonly causes emotional and allocation of attention disorders.
Psychiatric syndromes caused by infectious disease most commonly include depression, OCD, panic disorder, social phobias, variants of ADD, episodic impulsive hostility, bipolar disorders, eating disorders, dementia, various cognitive impairments, psychosis, and a few cases of dissociative episodes.
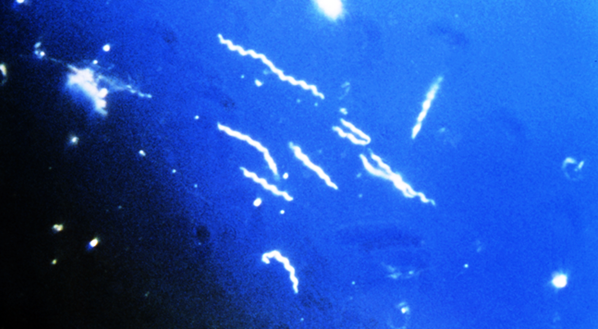
In clinical experience, the link between infectious disease and psychopathology has been an issue with Lyme disease, syphilis, babesiosis, ehrlichiosis, mycoplasma pneumonia, toxoplasmosis; stealth virus, borna virus, AIDS, CMV; herpes, strep and other unknown infectious agents. In the collective database of patients demonstrating psychiatric symptoms in response to infectious disease, the majority of the cases has been infected by ticks. Aristotle referred to ticks as "filthy disgusting animals" (1). They spend their lives living in dirt, feeding on the blood of mice, rats, and other wild animals (2). When they bite humans, they pose a risk of injecting an infectious cocktail of pathogens into the host.
Patients with psychiatric symptoms from tick-borne diseases are most commonly infected by Borrelia burgdorferi, (Bb) the causative agent of Lyme disease and quite often other coinfections-infections. There is an increasing recognition that many chronic relapsing infections are complex interactive infections in which microbes interact with each other in a manner that contributes to the disease process. The models most commonly discussed are coinfections associated with HIV and tick-borne coinfections. For example, coinfections associated with Lyme disease may be acquired at the same time, before or after the Bb infection. Interactive infections, however, is a more accurate term than coinfections, since these infections invariably cause an interaction that changes the disease process.
To understand coinfections, we need to begin by defining each disease separately. This, of course, is an area of much controversy in regard to late stage chronic relapsing Lyme disease. A similar controversy exists in regard to other chronic infections. It is difficult to explain how interaction occurs when there is such disagreement defining the clinical syndrome and pathophysiology associated with each infection separately.
A couple of years ago, other tick-borne diseases were not considered to be very significant in contributing to chronic, relapsing Lyme disease. Once there was a greater focus upon these organisms, it became clear that coinfections were a significant issue. We can better understand chronic, relapsing diseases such as Lyme disease by taking a closer look at interactive coinfections, host vulnerability, and host response that contributes to the disease process.
Some very interesting work is being done to better understand the role of interactive coinfections between Bb and stealth virus, Candida, Babesia, and Ehrlichia. For example, stealth virus facilitates lipid production which facilitates Bb growth (3), Bb is protected from host defenses inside Candida cells (4), Babesia causes immunosupression, and Ehrlichia causes bone marrow suppression.
In summary, the complexities of these issues teach us humility. To better understand the clinical syndrome associated with these infections, internists need to recognize the significance of mental symptoms in chronic interactive infections and psychiatrists need to better appreciate the role of microbes in causing mental illness.
Sources:
We lead our entire lives surrounded by microbes. In a state of health, there is a balance, a reasonable resistance to infectious disease, and a peaceful co-existence. In contrast, with infectious disease, there is an imbalance between the threat posed by microbes and host defenses. This balance is affected by environmental factors (including exposure to pathogens) and a number of host factors such as genetics and/or increased vulnerability as a result of a state of chronic stress. Although the stress response is adaptive in a short time frame to allocate resources during a crisis, if the stress response is persistent, rather than cyclic, it further increases vulnerability to disease.
The most common sequence of disease begins with a vulnerability and an exposure to one or more stressors. The vulnerability may commonly include genetic and/or increased vulnerability as a result of chronic stress. As a result of these and other vulnerabilities, the microbe more easily penetrates the host's defenses and an initial infection may then occur.
Although infection may occur from microbes that are always present in the environment, a greater number of organisms or more virulent organisms further increase risk. Acute infections are most noteworthy in general medicine. However, the course of the infection most relevant to psychiatry includes injury from a prior infection; chronic, low-grade, persistent relapsing infections; or the persistence of the infectious agent in the inactive state. When persistent, relapsing infection occurs, there may be extended period of latency followed by some triggering event(s) (i.e.: chronic stress, injury, surgery, or other infectious agents), which may then cause the activation of the infectious agent(s) and the progression of the pathological process.
Some injury in infectious disease is a result of toxic products or direct cell injury, but a significant amount of injury is a result of host defenses gone awry in response to the infection. Neural injury may occur by a variety of mechanisms, which include vasculitis, direct cell injury, toxins, inflammation, cytokines, autoimmune mechanisms, incorporation of parasite DNA into host DNA, and excitotoxicity. This injury leads to a vicious cycle of disease, resulting in dysfunction of associative and/or modulating centers of the brain. Injury to associative centers more commonly causes cognitive symptoms, while injury to modulating centers more commonly causes emotional and allocation of attention disorders.
Psychiatric syndromes caused by infectious disease most commonly include depression, OCD, panic disorder, social phobias, variants of ADD, episodic impulsive hostility, bipolar disorders, eating disorders, dementia, various cognitive impairments, psychosis, and a few cases of dissociative episodes.
In clinical experience, the link between infectious disease and psychopathology has been an issue with Lyme disease, syphilis, babesiosis, ehrlichiosis, mycoplasma pneumonia, toxoplasmosis; stealth virus, borna virus, AIDS, CMV; herpes, strep and other unknown infectious agents. In the collective database of patients demonstrating psychiatric symptoms in response to infectious disease, the majority of the cases has been infected by ticks. Aristotle referred to ticks as "filthy disgusting animals" (1). They spend their lives living in dirt, feeding on the blood of mice, rats, and other wild animals (2). When they bite humans, they pose a risk of injecting an infectious cocktail of pathogens into the host.
Patients with psychiatric symptoms from tick-borne diseases are most commonly infected by Borrelia burgdorferi, (Bb) the causative agent of Lyme disease and quite often other coinfections-infections. There is an increasing recognition that many chronic relapsing infections are complex interactive infections in which microbes interact with each other in a manner that contributes to the disease process. The models most commonly discussed are coinfections associated with HIV and tick-borne coinfections. For example, coinfections associated with Lyme disease may be acquired at the same time, before or after the Bb infection. Interactive infections, however, is a more accurate term than coinfections, since these infections invariably cause an interaction that changes the disease process.
To understand coinfections, we need to begin by defining each disease separately. This, of course, is an area of much controversy in regard to late stage chronic relapsing Lyme disease. A similar controversy exists in regard to other chronic infections. It is difficult to explain how interaction occurs when there is such disagreement defining the clinical syndrome and pathophysiology associated with each infection separately.
A couple of years ago, other tick-borne diseases were not considered to be very significant in contributing to chronic, relapsing Lyme disease. Once there was a greater focus upon these organisms, it became clear that coinfections were a significant issue. We can better understand chronic, relapsing diseases such as Lyme disease by taking a closer look at interactive coinfections, host vulnerability, and host response that contributes to the disease process.
Some very interesting work is being done to better understand the role of interactive coinfections between Bb and stealth virus, Candida, Babesia, and Ehrlichia. For example, stealth virus facilitates lipid production which facilitates Bb growth (3), Bb is protected from host defenses inside Candida cells (4), Babesia causes immunosupression, and Ehrlichia causes bone marrow suppression.
In summary, the complexities of these issues teach us humility. To better understand the clinical syndrome associated with these infections, internists need to recognize the significance of mental symptoms in chronic interactive infections and psychiatrists need to better appreciate the role of microbes in causing mental illness.
Sources:
- Adapted from Burrascano, J., The New Lyme Disease Diagnostic Hints and Treatment Guidelines for Tick-Borne Illness, l2th Edition, copyright 10/98.
- Burgdorfer, W.B., Increased Evidence of Mosquito/Spirochete Associations; 11th International Scientific Conference on Lyme Disease and other Spirochetal & Tick-Borne Disorders.
- Discussion with Dr. John Martin
- Discussion with Dr. Linda Mattman
About the author
Dr. Robert Bransfield, MD is a psychiatrist specializing in the link between mental health and microbes. You can learn more by visiting Dr. Robert Bransfield's website mentalhealthandillness.com.
latest posts
tags
Disclaimer: The information on this website is not a substitute for professional medical advice.
Always consult with your treating physician before altering any treatment protocol.
Always consult with your treating physician before altering any treatment protocol.