Manuka Honey as Medicine
September 30, 2014 in Herbs/Natural Remedies by Peter Molan, MD
Honey is one of the oldest known medicines, its recorded use (for the treatment of wounds and eye infections) dates back four-thousand years [1]. Unlike most other ancient medicines, it is still widely used. It was commonly used as a wound treatment, until it was replaced by antibiotics in the 1940's. With the ever-growing antibiotic resistant bacteria strains becoming a world-wide problem, there has been a revival in the use of honey to treat infected wounds. Two review articles published in medical journals [2,3] summarize the 33 randomized controlled trials (RCTs) of honey in wound care published up to 2011, with a total of 3,556 participants in the trials. The trials provide a large body of evidence for the effectiveness of honey as a treatment for a wide range of wounds and for burns. One of these reviews [3] also summarizes evidence from laboratory studies that provide scientific rationale for the effectiveness of honey as a wound treatment. As well as providing a moist environment that is optimal for repaired tissue to grow, honey has bioactivities which stimulate the production of cell growth factors, stop inflammation which would otherwise prevent healing, and kill infectious bacteria.
Honey has a very broad spectrum of activity as an antimicrobial agent [4]. Although most published studies have not used standardized honeys (the potency of the antimicrobial activity can vary as much as 100-fold), there have been several studies conducted with honeys selected to have a median level of antibacterial activity. These have measured the sensitivity of the major wound-infecting species of bacteria to honey [8]. It has been found that even with the most resistant strains, a honey with a median level of activity can be diluted at least 10-fold and will still stop the growth of bacteria. All of the various species of “superbugs” that can no longer be treated with antibiotics are just as sensitive to honey as are the strains of these species that have not yet developed a resistance.
Ancient Greek physicians were aware that some types of honey were better than others for medicinal use, and this knowledge has continued into present-day folk medicine around the world [5]. In New Zealand, folk knowledge is that manuka honey is the best type of honey to use as an antiseptic. Research proved this theory by revealing that manuka honey has an antibacterial activity that is different in nature from other honeys [6]. In all other types of honey, antibacterial activity is primarily due to hydrogen peroxide that is produced by the enzyme activity in honey when it is diluted [4]. When an enzyme (catalase) was added to completely destroy any hydrogen peroxide produced in the solutions of various honeys tested, it was found that whereas all other honeys lost their antibacterial activity, the high level of antibacterial activity in manuka honey was fully retained. Subsequent research investigating a very large number of types of honey in various countries has shown that this unusual type of antibacterial activity, termed ‘non-peroxide activity’, is unique to manuka honey. However, it does occur in honey from some closely related species of Leptospermum trees that grow in restricted locations in Australia. The non-peroxide antibacterial activity is now known to be a result of the methylglyoxal that manuka honey forms from dihydroxyacetone, a characteristic uniquely to manuka nectar.
The medical potential of this non-peroxide activity was realized from the outset. The cells of animal tissues contain a high level of the enzyme catalase which destroys hydrogen peroxide, a process seen when a hydrogen peroxide solution is applied on a cut as an antiseptic. The fizzing seen is due to catalase activity rapidly converting the solution from hydrogen peroxide to water and oxygen. Although in laboratory testing some other types of honey may be found to have more potent antibacterial activity than manuka honey, on an open wound most of the antibacterial activity of honeys other than manuka honey will be destroyed by catalase. Manuka honey, on the other hand, will retain its full activity. In one of my YouTube videos, titled “Why you need the right sort of activity in manuka honey,” honeys are compared with and without some blood included in the bacterial growth medium. A sample of honey with hydrogen peroxide activity that is far more potent than the non-peroxide activity of a sample of manuka honey shows no visible antibacterial activity when there is 1% blood is present. In saliva there is a similar enzyme, lactoperoxidase, which also destroys hydrogen peroxide, thus decreasing the relative usefulness of honeys other than manuka honey for treating oral infections.
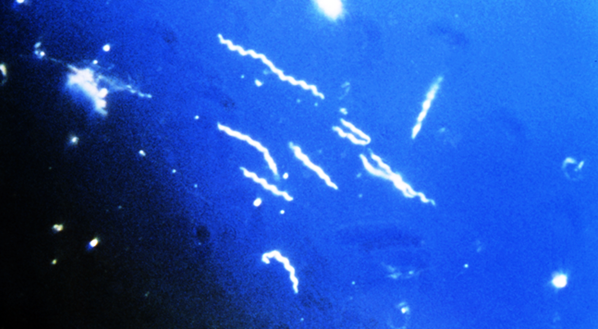
Another medically useful feature of the unique type of antibacterial activity in manuka honey is its ability to penetrate biofilms. It is becoming increasingly apparent that the bacteria in chronically infected wounds grow biofilms on the wound tissues. The gummy matrix of these films prevents antibiotics from penetrating the infected wounds, and prevents the body’s own antibacterial defenses from reaching and killing the bacteria as well.
A very important activity of honey in wound treatment is its anti-inflammatory action. When a wound is not healing, it is because inflammation is preventing the healing process from occurring. If there is severe inflammation the tissues can be eroded, allowing ulcers to develop. With burn injuries, which cause a large amount of inflammation, the erosion from the inflammation can cause more damage than the heat did. Clinical trials of honey on burn injuries show that honey is very effective in preventing this type of ongoing damage.
Research has found an explanation for the mechanism of action of the anti-inflammatory activity of honey [7]. It suppresses the responsiveness of leukocytes, which detect and engulf bacteria and damaged tissue, triggering a cascade of reactions from the body’s inflammatory response to infection or tissue damage. Thus, honey's ability to suppress the responsiveness of leukocytes tones down the severity of inflammation. Research has identified the component of honey responsible for this action, a protein called Apalbumin-1 which bees add to the nectar that they harvest to produce honey. It was found that in manuka honey, the methylglyoxal present reacts with Apalbumin-1 by modifying it in a manner that makes it more potent in suppressing the inflammatory response. This gives manuka honey a more potent anti-inflammatory activity than those of other types of honey.
Of the eight honey wound-care products on sale that are registered with regulatory authorities such as the FDA as medical devices, and the two registered for use in veterinary medicine, seven are manufactured using manuka honey. Modern medicine is currently developing other medicinal uses of honey, besides its use to treat wounds. Such uses include treatment for eye infections, ear infections, nasal sinus infections, gum disease, lung infections with honey inhaled from a nebulizer, and suppression of tissue damage from radiation burns obtained during radiotherapy treatment for cancer. In most of these new developments, manuka honey is being used in the clinical evaluation of the effectiveness of honey.
Consumer demand for manuka honey has greatly increased, as more people have become aware of its unusual antibacterial activity. As a consequence, the price of manuka honey has spiked. This has unfortunately led to a lot of exploitation of consumers by some marketers falsely labelling what is sold. They also exploit consumers who do not realize the activity rated on the label is not the type of activity that is unique to manuka honey, but is due to hydrogen peroxide and thus is no different from that in much cheaper honey from other floral sources. Consumers need to verify from the producer, as opposed to the sales counter assistant, that the rated antibacterial activity is definitely non-peroxide activity or that the content of methylglyoxal is stated. To be confident that a honey is at least 50% from manuka nectar, and thus can be legitimately called manuka honey, the rating of non-peroxide activity should be at least 10 (i.e. is equivalent in antibacterial potency to a 10% solution of the reference standard antiseptic phenol), or the methylglyoxal content should be stated to be at least 250 mg/kg.
References
1. Molan PC (1999) Why honey is effective as a medicine. 1. Its use in modern medicine. Bee World 80: 80-92.
2. Molan PC (2006) The evidence supporting the use of honey as a wound dressing. The International Journal of Lower Extremity Wounds 5: 40-54.
3. Molan PC (2011) The evidence and the rationale for the use of honey as a wound dressing. Wound Practice and Research (Journal of the Australian Wound Management Association) 19: 204-221.
4. Molan PC (1992) The antibacterial activity of honey. 1. The nature of the antibacterial activity. Bee World 73: 5-28.
5. Molan PC (1992) The antibacterial activity of honey. 2. Variation in the potency of the antibacterial activity. Bee World 73: 59-76.
6. Allen KL, Molan PC & Reid GM (1991) A survey of the antibacterial activity of some New Zealand honeys. Journal of Pharmacy and Pharmacology 43: 817-822.
7. Bean A (2012) Investigating the anti-inflammatory activity of honey. PhD Thesis, University of Waikato http://hdl.handle.net/10289/6218.
8.https://www.academia.edu/2189571/Pdf_6_The_antibacterial_activity_of_honey_and_its_role_in_treating_diseases ).
The full text of these papers is available free of charge from the University of Waikato Research Commons: http://researchcommons.waikato.ac.nz/browse?value=Molan%2C+Peter+C.&
Resources
A large amount of educational material about the therapeutic properties of honey is available on http://waikato.academia.edu/PeterMolan/Papers. The website also has articles on dressing wounds with honey and details of honey wound-care products registered as medical products with the FDA. It also has articles about the unusual antibacterial activity of manuka honey and how the level of this activity is measured and rated on jars of manuka honey on sale.
Honey has a very broad spectrum of activity as an antimicrobial agent [4]. Although most published studies have not used standardized honeys (the potency of the antimicrobial activity can vary as much as 100-fold), there have been several studies conducted with honeys selected to have a median level of antibacterial activity. These have measured the sensitivity of the major wound-infecting species of bacteria to honey [8]. It has been found that even with the most resistant strains, a honey with a median level of activity can be diluted at least 10-fold and will still stop the growth of bacteria. All of the various species of “superbugs” that can no longer be treated with antibiotics are just as sensitive to honey as are the strains of these species that have not yet developed a resistance.
Ancient Greek physicians were aware that some types of honey were better than others for medicinal use, and this knowledge has continued into present-day folk medicine around the world [5]. In New Zealand, folk knowledge is that manuka honey is the best type of honey to use as an antiseptic. Research proved this theory by revealing that manuka honey has an antibacterial activity that is different in nature from other honeys [6]. In all other types of honey, antibacterial activity is primarily due to hydrogen peroxide that is produced by the enzyme activity in honey when it is diluted [4]. When an enzyme (catalase) was added to completely destroy any hydrogen peroxide produced in the solutions of various honeys tested, it was found that whereas all other honeys lost their antibacterial activity, the high level of antibacterial activity in manuka honey was fully retained. Subsequent research investigating a very large number of types of honey in various countries has shown that this unusual type of antibacterial activity, termed ‘non-peroxide activity’, is unique to manuka honey. However, it does occur in honey from some closely related species of Leptospermum trees that grow in restricted locations in Australia. The non-peroxide antibacterial activity is now known to be a result of the methylglyoxal that manuka honey forms from dihydroxyacetone, a characteristic uniquely to manuka nectar.
The medical potential of this non-peroxide activity was realized from the outset. The cells of animal tissues contain a high level of the enzyme catalase which destroys hydrogen peroxide, a process seen when a hydrogen peroxide solution is applied on a cut as an antiseptic. The fizzing seen is due to catalase activity rapidly converting the solution from hydrogen peroxide to water and oxygen. Although in laboratory testing some other types of honey may be found to have more potent antibacterial activity than manuka honey, on an open wound most of the antibacterial activity of honeys other than manuka honey will be destroyed by catalase. Manuka honey, on the other hand, will retain its full activity. In one of my YouTube videos, titled “Why you need the right sort of activity in manuka honey,” honeys are compared with and without some blood included in the bacterial growth medium. A sample of honey with hydrogen peroxide activity that is far more potent than the non-peroxide activity of a sample of manuka honey shows no visible antibacterial activity when there is 1% blood is present. In saliva there is a similar enzyme, lactoperoxidase, which also destroys hydrogen peroxide, thus decreasing the relative usefulness of honeys other than manuka honey for treating oral infections.
Another medically useful feature of the unique type of antibacterial activity in manuka honey is its ability to penetrate biofilms. It is becoming increasingly apparent that the bacteria in chronically infected wounds grow biofilms on the wound tissues. The gummy matrix of these films prevents antibiotics from penetrating the infected wounds, and prevents the body’s own antibacterial defenses from reaching and killing the bacteria as well.
A very important activity of honey in wound treatment is its anti-inflammatory action. When a wound is not healing, it is because inflammation is preventing the healing process from occurring. If there is severe inflammation the tissues can be eroded, allowing ulcers to develop. With burn injuries, which cause a large amount of inflammation, the erosion from the inflammation can cause more damage than the heat did. Clinical trials of honey on burn injuries show that honey is very effective in preventing this type of ongoing damage.
Research has found an explanation for the mechanism of action of the anti-inflammatory activity of honey [7]. It suppresses the responsiveness of leukocytes, which detect and engulf bacteria and damaged tissue, triggering a cascade of reactions from the body’s inflammatory response to infection or tissue damage. Thus, honey's ability to suppress the responsiveness of leukocytes tones down the severity of inflammation. Research has identified the component of honey responsible for this action, a protein called Apalbumin-1 which bees add to the nectar that they harvest to produce honey. It was found that in manuka honey, the methylglyoxal present reacts with Apalbumin-1 by modifying it in a manner that makes it more potent in suppressing the inflammatory response. This gives manuka honey a more potent anti-inflammatory activity than those of other types of honey.
Of the eight honey wound-care products on sale that are registered with regulatory authorities such as the FDA as medical devices, and the two registered for use in veterinary medicine, seven are manufactured using manuka honey. Modern medicine is currently developing other medicinal uses of honey, besides its use to treat wounds. Such uses include treatment for eye infections, ear infections, nasal sinus infections, gum disease, lung infections with honey inhaled from a nebulizer, and suppression of tissue damage from radiation burns obtained during radiotherapy treatment for cancer. In most of these new developments, manuka honey is being used in the clinical evaluation of the effectiveness of honey.
Consumer demand for manuka honey has greatly increased, as more people have become aware of its unusual antibacterial activity. As a consequence, the price of manuka honey has spiked. This has unfortunately led to a lot of exploitation of consumers by some marketers falsely labelling what is sold. They also exploit consumers who do not realize the activity rated on the label is not the type of activity that is unique to manuka honey, but is due to hydrogen peroxide and thus is no different from that in much cheaper honey from other floral sources. Consumers need to verify from the producer, as opposed to the sales counter assistant, that the rated antibacterial activity is definitely non-peroxide activity or that the content of methylglyoxal is stated. To be confident that a honey is at least 50% from manuka nectar, and thus can be legitimately called manuka honey, the rating of non-peroxide activity should be at least 10 (i.e. is equivalent in antibacterial potency to a 10% solution of the reference standard antiseptic phenol), or the methylglyoxal content should be stated to be at least 250 mg/kg.
References
1. Molan PC (1999) Why honey is effective as a medicine. 1. Its use in modern medicine. Bee World 80: 80-92.
2. Molan PC (2006) The evidence supporting the use of honey as a wound dressing. The International Journal of Lower Extremity Wounds 5: 40-54.
3. Molan PC (2011) The evidence and the rationale for the use of honey as a wound dressing. Wound Practice and Research (Journal of the Australian Wound Management Association) 19: 204-221.
4. Molan PC (1992) The antibacterial activity of honey. 1. The nature of the antibacterial activity. Bee World 73: 5-28.
5. Molan PC (1992) The antibacterial activity of honey. 2. Variation in the potency of the antibacterial activity. Bee World 73: 59-76.
6. Allen KL, Molan PC & Reid GM (1991) A survey of the antibacterial activity of some New Zealand honeys. Journal of Pharmacy and Pharmacology 43: 817-822.
7. Bean A (2012) Investigating the anti-inflammatory activity of honey. PhD Thesis, University of Waikato http://hdl.handle.net/10289/6218.
8.https://www.academia.edu/2189571/Pdf_6_The_antibacterial_activity_of_honey_and_its_role_in_treating_diseases ).
The full text of these papers is available free of charge from the University of Waikato Research Commons: http://researchcommons.waikato.ac.nz/browse?value=Molan%2C+Peter+C.&
Resources
A large amount of educational material about the therapeutic properties of honey is available on http://waikato.academia.edu/PeterMolan/Papers. The website also has articles on dressing wounds with honey and details of honey wound-care products registered as medical products with the FDA. It also has articles about the unusual antibacterial activity of manuka honey and how the level of this activity is measured and rated on jars of manuka honey on sale.
About the author
latest posts
tags
Disclaimer: The information on this website is not a substitute for professional medical advice.
Always consult with your treating physician before altering any treatment protocol.
Always consult with your treating physician before altering any treatment protocol.